(Valelopardo / Pixabay)
(Valelopardo / Pixabay)
A new study has found cannabidiol, a product of the cannabis plant also known as CBD, can block COVID-19 infection in human cells and in mice.
Scientists say the discovery means more research is warranted, including a full human trial measuring CBD’s effectiveness against COVID-19. While the findings are positive, they advise against using commercially available CBD products, which can vary in potency and quality, as a treatment for COVID-19
The study was published Jan. 20 in Science Advances. It involved treating human cells and mice with CBD to test its effect on COVID-19, as well an analysis more than 1,000 individuals taking a medically prescribed, FDA-approved formulation of CBD for the treatment of epilepsy.
“This does not mean (an individual) should run out and get CBD products from a local dispensary or favorite bakery for a CBD muffin or CBD gummy bears,” said Marsha Rosner, a professor at the University of Chicago and a senior author of the study. “We were very careful to use very high purity, very high-quality CBD.”
The study showed CBD can block the virus from replicating in human cells after entering those cells, “which is important because it has the potential to be used as an early response agent, not just for prevention,” said Rosner. “CBD works on our cells after the virus enters – it’s not targeting the virus directly. What it’s doing is activating one of our own systems to respond to pathogens.”
By not targeting the virus directly, researchers believe CBD should be effective against COVID-19 variants, which attempt to evade the immune system, according to Rosner, who said research found it to be effective against the alpha, beta and gamma variants as well as the original strain.
Researchers plan to investigate its efficacy against the delta and omicron variants.
The study also found CBD given to mice before infection decreased the amount of virus in their lungs and nasal passages, which shows it has the potential to work in humans, said Rosner. “These results provide major support for a clinical trial of CBD in humans.”
The analysis of a group of individuals taking a medically prescribed formulation of CBD for epilepsy found patients tested positive for COVID-19 at significantly lower rates than patients from similar demographic backgrounds who were not taking CBD.
“We don’t know yet if CBD can prevent COVID-19, but the results provide strong evidence for a clinical trial such as those that were done for vaccines to see if CBD is effective for preventing or decreasing COVID-19 infection,” Rosner said. “We do not view CBD as a substitute for vaccines or masking, or any of the other guidelines the CDC has suggested. We should think of this as another tool in our arsenal. We imagine if we find it works in clinical trial, it might be useful for breakthrough infections.”
The findings about CBD were not found in marijuana, which is also derived from the cannabis plant.
“We can pretty definitively say smoking marijuana is not going to help you fight COVID-19,” Rosner said, adding the tetrahydrocannabinol or THC in marijuana that gets people high actually decreased the efficacy of CBD against COVID-19.
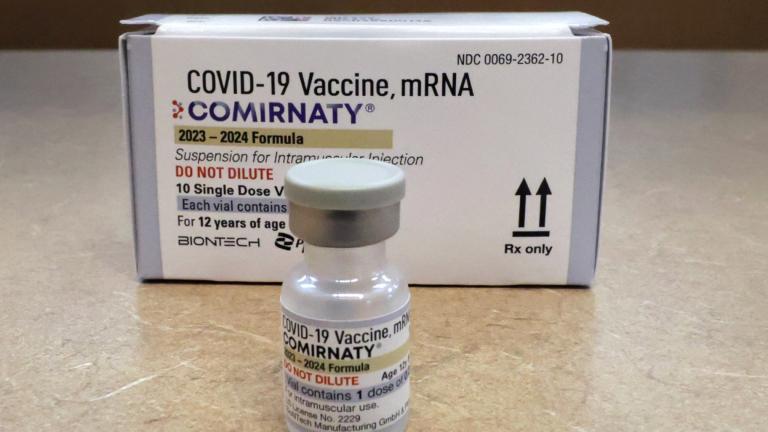
Current COVID-19 treatments
While researchers are investigating potential clinical trials to further analyze CBD’s effect on COVID-19, there are treatment options available for COVID-19, including antiviral pills that can be taken at home.
“There’s no cure at this point. What we have are medications that studies have shown decrease the risk of progression to severe disease or hospitalization in high-risk patients,” said Dr. Shivanjali Shankaran, an infectious disease specialist at Rush University Medical Center.
The two antiviral drugs currently available – one made by Pfizer (Paxlovid) and another made by Merck (Molnupiravir) – are intended for people with mild or moderate COVID-19 who are more likely to become seriously ill. That includes people with diabetes, heart disease, liver problems and other conditions that make people more vulnerable, according to Shankaran.
People need to inform their providers of all medications and supplements they’re taking due to potential drug interactions, says Dr. Susan Bleasdale, medical director and chief quality officer at UI Health. There are no known drug interactions for Molnupiravir based on limited available data, while certain drugs are associated with serious and/or life-threatening reactions for Paxlovid, according to the U.S. Food and Drug Administration’s emergency use authorization fact sheets for the respective medications. Molnupiravir isn’t recommended for pregnant people because of the potential for birth defects, which means people need to use contraception while taking it, according to Bleasdale.
While both drugs have shown to be effective, they are only available via prescription and must be taken as soon as possible once symptoms begin. “Time is of the essence,” said Shankaran.
Illinois has started receiving shipments of both medications, but supplies are limited, which means not everyone who wants them can receive them.
“The oral antiviral medications we have are super promising,” said Dr. Emily Landon, an infectious disease specialist at UChicago Medicine. “Once they’re available in reasonable quantities, they can change the way we mange COVID-19.”
Monoclonal antibodies are another treatment option intended to prevent severe disease and death by supplying concentrated doses of antibodies early in an infection.
People who have medical conditions that put them at higher risk of severe disease despite being vaccinated, as well as those who are unvaccinated, can benefit from these treatments, according to Bleasdale, if treatments are started early.
“By the time someone is coming into the hospital, it has no benefit and there may be some potential harm in inhibiting the immune system,” she said. “We want to save lives, and this is a treatment if you’re not vaccinated that can potentially save your life.”
But unlike the antivirals, they must be administered via an infusion.
“They can be used not only to treat infection, but also to prevent infection,” Landon said. “There are a number of different ones on the market that are really tailored to (COVID-19’s) spike protein. … The problem with monoclonal antibodies made for delta and the original strain of COVID is that they don’t work that well for omicron.”
That led the FDA to revoke emergency authorization for antibody drugs from Regeneron and Eli Lilly.
In its decision, the FDA said that omicron accounts for more than 99% of infections in the U.S., making it “highly unlikely” the antibodies would help people seeking treatment. But if the drugs prove effective against future variants, the FDA said it could reauthorize their use.
There are other monoclonal antibodies (Sotrovimab and Evusheld) that appear to be effective against omicron, according to clinicians. But they too are in short supply and are limited to those with mild to moderate symptoms who are most at risk of developing severe illness. To help individuals locate where to find approved treatments, the Illinois Department of Public Health maintains an online database of places providing them.
Another treatment option is remdesivir – the first drug approved for COVID-19. Originally limited to hospitalized patients, the FDA recently expanded the antiviral’s approval to include adults and children with early COVID-19 who are at high risk of hospitalization.
While remdesivir is widely available, it requires three consecutive IV infusions over three days, presenting challenges to both patients and providers. “Hospitals are too full to admit people,” Landon said. That means an individual would have to make three separate trips to a hospital or infusion center to receive treatment.
Even with these treatment options, clinicians stressed the need for vaccination.
“The most important thing is to get vaccinated – vaccinated and boosted,” said Shankaran, who urged people to get tested early if they develop symptoms and to talk with their providers about potential treatment options.
Bleasdale agreed.
“I’ve been asked by others, ‘Is this going to replace vaccination?’ No, it’s not,” she said, adding the vaccines still prevented hospitalizations and deaths during the omicron surge.
And people shouldn’t be tossing out their masks just yet, according to Landon.
“We’re not done yet. It’s going to be OK, but now is not the time to stop our mitigations just yet,” she said.
The Associated Press contributed.
Note: An earlier version of this story incorrectly identified drug interactions for antiviral medications. The story has been updated.
Contact Kristen Thometz: @kristenthometz | (773) 509-5452 | [email protected]